Intro
Streamline wound care with a printable wound assessment form, featuring detailed wound measurement, tissue classification, and treatment planning, ideal for healthcare professionals to track wound healing progress and improve patient outcomes.
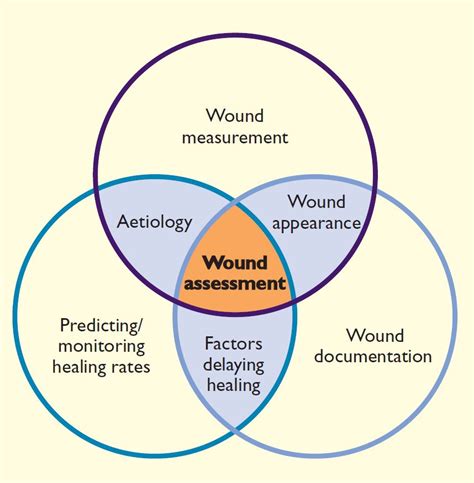
The importance of wound assessment cannot be overstated, as it plays a crucial role in the healing process of patients suffering from various types of wounds. A thorough assessment helps healthcare professionals to identify the type and severity of the wound, develop an effective treatment plan, and monitor the patient's progress. One essential tool used in wound assessment is the printable wound assessment form. This form provides a standardized framework for collecting and documenting relevant information about the wound, enabling healthcare professionals to make informed decisions and provide high-quality care.
Wound assessment is a complex process that involves evaluating various factors, including the wound's size, shape, location, and depth. It also requires assessing the patient's overall health, medical history, and any underlying conditions that may affect the healing process. By using a printable wound assessment form, healthcare professionals can ensure that they collect all the necessary information, reducing the risk of errors or oversights. Moreover, the form helps to facilitate communication among healthcare team members, ensuring that everyone involved in the patient's care is aware of the wound's status and the treatment plan.
The use of printable wound assessment forms has become increasingly popular in recent years, as they offer several benefits over traditional methods of documentation. For one, they provide a standardized framework for collecting and documenting information, which helps to reduce errors and inconsistencies. Additionally, the forms can be easily customized to meet the specific needs of individual patients or healthcare facilities, making them a versatile tool for wound assessment. Furthermore, the forms can be used in conjunction with electronic health records, enabling healthcare professionals to access and update patient information quickly and efficiently.
Benefits of Using a Printable Wound Assessment Form
The benefits of using a printable wound assessment form are numerous. Some of the most significant advantages include:
- Improved accuracy and consistency in wound documentation
- Enhanced communication among healthcare team members
- Increased efficiency in collecting and documenting wound information
- Better patient outcomes due to more effective treatment plans
- Reduced risk of errors or oversights in wound care
- Customizable to meet the specific needs of individual patients or healthcare facilities
Components of a Comprehensive Wound Assessment Form
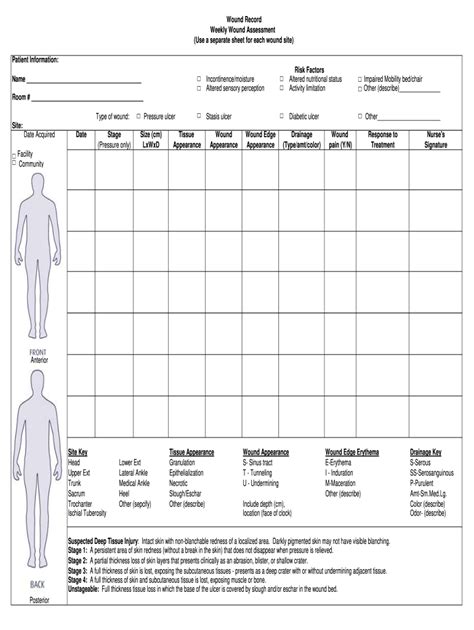
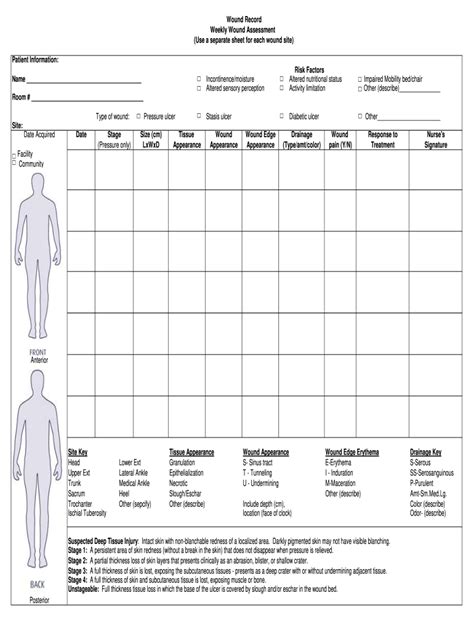
A comprehensive wound assessment form should include several key components, such as:- Patient demographics and medical history
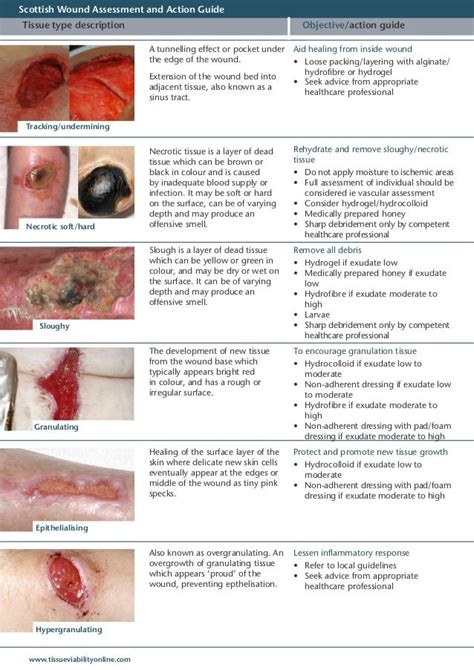
- Wound location, size, shape, and depth
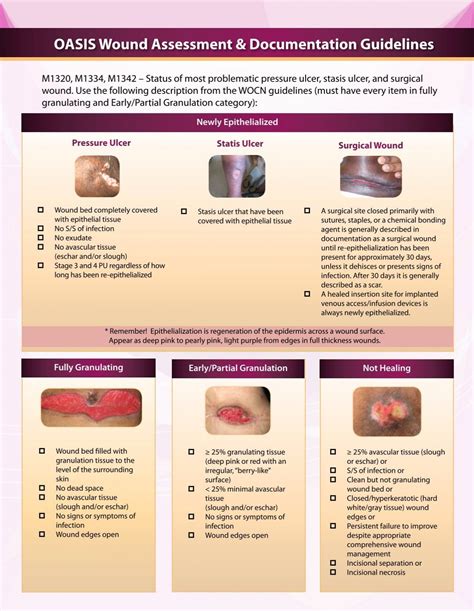
- Wound type (e.g., pressure ulcer, diabetic foot ulcer, surgical wound)
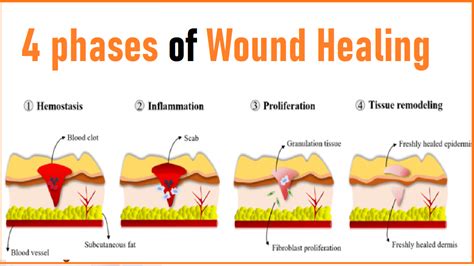
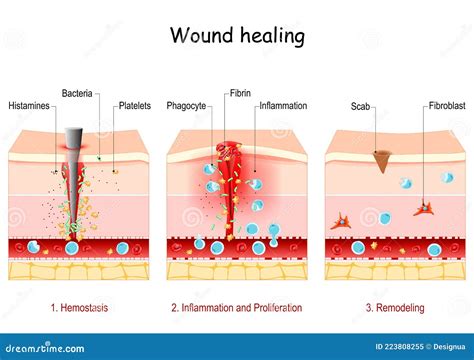
- Wound stage (e.g., stage 1, stage 2, stage 3, stage 4)
- Presence of any underlying conditions that may affect healing (e.g., diabetes, peripheral artery disease)
- Current treatments and medications
- Nutritional status and dietary habits
- Mobility and activity level
- Pain assessment and management plan
How to Use a Printable Wound Assessment Form

Using a printable wound assessment form is a straightforward process. Here are the steps to follow:
- Download and print the form: Obtain a copy of the wound assessment form and print it on paper or use an electronic version.
- Complete the patient demographics section: Fill in the patient's name, date of birth, medical record number, and other relevant demographic information.
- Assess the wound: Evaluate the wound's location, size, shape, and depth, and document this information on the form.
- Determine the wound stage: Use the wound staging guidelines to determine the stage of the wound and document this information on the form.
- Complete the rest of the form: Fill in the remaining sections of the form, including the patient's medical history, current treatments and medications, nutritional status, and mobility and activity level.
- Review and update the form regularly: Review the form regularly and update it as necessary to reflect changes in the patient's condition or treatment plan.
Best Practices for Wound Assessment and Documentation
To ensure accurate and effective wound assessment and documentation, follow these best practices:- Use a standardized wound assessment form to collect and document information
- Assess the wound regularly and update the documentation as necessary
- Take clear and concise photographs of the wound to document its progress
- Use a wound measurement tool to accurately measure the wound's size and depth
- Document any changes in the wound's appearance, size, or depth
- Communicate effectively with other healthcare team members to ensure everyone is aware of the patient's wound status and treatment plan
Common Challenges in Wound Assessment and Documentation
Despite the importance of wound assessment and documentation, several challenges can arise. Some of the most common challenges include:
- Inaccurate or incomplete documentation
- Lack of standardization in wound assessment and documentation
- Insufficient communication among healthcare team members
- Limited access to wound care resources and expertise
- High patient volume and limited time for wound assessment and documentation
Strategies for Overcoming Challenges in Wound Assessment and Documentation
To overcome the challenges in wound assessment and documentation, consider the following strategies:- Implement a standardized wound assessment form and documentation process
- Provide education and training on wound assessment and documentation for healthcare staff
- Increase communication among healthcare team members through regular meetings and updates
- Develop a wound care team with specialized expertise and resources
- Use technology, such as electronic health records and mobile apps, to streamline wound assessment and documentation
Future Directions in Wound Assessment and Documentation

The field of wound assessment and documentation is constantly evolving, with new technologies and innovations emerging regularly. Some of the future directions in wound assessment and documentation include:
- Increased use of artificial intelligence and machine learning in wound assessment and documentation
- Development of mobile apps and digital platforms for wound assessment and documentation
- Integration of wound assessment and documentation with electronic health records and other healthcare systems
- Use of advanced imaging technologies, such as 3D scanning and photography, to document wound progress
- Increased focus on patient-centered care and patient engagement in wound assessment and documentation
Conclusion and Final Thoughts
In conclusion, printable wound assessment forms are a valuable tool in wound care, providing a standardized framework for collecting and documenting relevant information about the wound. By using these forms, healthcare professionals can ensure accurate and effective wound assessment and documentation, leading to better patient outcomes and improved wound healing. As the field of wound care continues to evolve, it is essential to stay up-to-date with the latest technologies and innovations in wound assessment and documentation.Wound Assessment Image Gallery



What is a wound assessment form?
+A wound assessment form is a standardized document used to collect and document information about a patient's wound, including its location, size, shape, and depth, as well as the patient's medical history and current treatments.
Why is wound assessment important?
+Wound assessment is important because it helps healthcare professionals to identify the type and severity of the wound, develop an effective treatment plan, and monitor the patient's progress, leading to better patient outcomes and improved wound healing.
How often should a wound be assessed?
+A wound should be assessed regularly, depending on the patient's condition and the wound's severity. Typically, wounds are assessed daily or weekly, but this may vary depending on the individual patient's needs.
We hope this article has provided you with valuable information about printable wound assessment forms and their importance in wound care. If you have any questions or comments, please don't hesitate to reach out to us. Share this article with your colleagues and friends who may be interested in learning more about wound assessment and documentation. Together, we can work towards improving patient outcomes and promoting better wound healing practices.
